Much like other companies around the world, we continue to monitor the outbreak of COVID-19 and assess what we can do as a firm to help the community around us. As experts in our field, we always seek to find new and better ways to serve our clients. Amid the current crisis, we have researched the best strategies for mitigating airborne virus contamination, specifically related to COVID-19.
Research conducted by Korea Centers for Disease Control has found that the structure of the virus is in the range of 0.1 microns, while HVAC filtration in patient care areas of hospitals utilize HEPA filters that are designed to capture/trap particles with 99.97% efficiency down to 0.3 microns in size. 1 This is 3 times bigger than the isolated virus – meaning the virus when not attached to a particle of water or mucus expelled by a symptomatic patient.
Other research by the University of California – Los Angeles2 and the American Society of Heating, Refrigerating, and Air Conditioning Engineers (ASHRAE)3 has found that air filtration is the most effective means of trapping particles of the virus, though not all of the virus in the air will be captured. In their position paper, ASHRAE recommends that air filtration with proper mixing of outside air (refer to ASHRAE Standards 62 and 170) is the best course of action by facilities to minimize exposure of airborne contaminants and organisms to building staff and healthcare workers.3
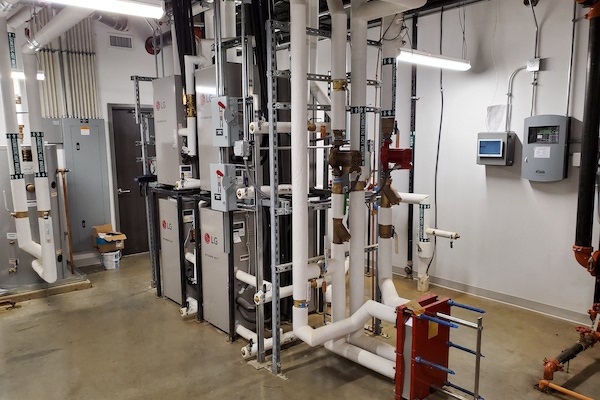
The UCLA research found that the virus will survive in the airstream for up to three (3) hours, while it will survive up to three (3) days on some solid surfaces.2 As a result, the primary mode of exposure to the virus has been through direct contact. Nonetheless, we cannot ignore the real risk of possible airborne spread of the virus, especially when healthcare workers are in the patient room. Negative pressure patient rooms can help prevent the airborne virus from traveling out into the common corridor or nurse stations. In retrofit applications like we might encounter in a pandemic, ASHRAE Standard 170 allows us to return air from Airborne Infectious Isolation patient rooms back to a central air handling unit (AHU) that is equipped with a high efficiency particulate arrestance (HEPA) filter in the final position of the unit. Supplying treated supply air from the air handling equipment at the front of the patient room, with return or exhaust air at the back of the room, will allow hospital staff to stand in front of the patient and be in the treated supply airstream that is then drawn across the patient and out of the room, instead of the other way around. Without exhausting the room where it is not practical, our challenge is to treat the air that is returned from the patient room back to the AHU.
Two methods are utilized today to offer additional treatment of building air beyond the traditional filter medias. First, ionization of air has been used to create an ozone field in buildings and spaces. When combined with activated or charged plates, particles in the air will be attracted to the plates and be pulled out of the air. Research supported by the Swedish Research Council on the use of this technology on viruses found that ionization of the air could draw as much as 37% of virus (influenza) out of the air and then render 97% of those virus molecules inactive. 4 The process took as long as 40 minutes but did have statistically significant results showing a 75% reduction in virus spread through airflow alone (no contact).
The second technology used to treat airstreams in buildings is ultraviolet radiation (UV-C and UVGI). For the purpose of quickest implementation, we only reviewed UVGI that is installed in the air handling equipment because it could be installed relatively quickly and would serve entire floors of a hospital, versus point-of-use products that could be installed in patient rooms at the ceiling level (upper-room) to treat air as it is being returned to the AHU. ASHRAE also found in their research that UVGI that is implemented at the ceiling level of patient rooms would be less effective in rooms where the air change rate is higher than six (6) air changes per hour (ACH) because the air (and any airborne virus) is drawn out of the room too quickly to be treated.3 In typical hospital design, we find that airflow in patient rooms can exceed 6 ACH.
Per the University of Washington, the only ways to kill the COVID-19 virus are soap (20 seconds of exposure will break down the virus), near boiling heat (more than what a human fever can achieve), and UV radiation.5 We then move to employing a UVGI bar in the air handling equipment to treat the air in the AHU at the filter media or downstream as the air passes over the cooling coils in the unit. The intensity of the UV radiation is increased in the unit to account for the short exposure time but is reported to kill as much as 100% of virus in the airstream. The technology has been utilized in hospitals since 1940. Research by a Harvard medical student in the 1950s and 1960s showed that he was able to inactivate the infected air by 100%.6 Using the same results, the student was able to reduce the airborne spread of influenza in a Veterans Hospital TB wing down from 18.9% to 1.9%.
Researchers have found that UV is most effective in preventing infections spread chiefly by droplet nuclei, not direct contact.6 Implementing UV techniques in the hospital will not solve our current pandemic but will greatly increase the safety for those that may be exposed through airborne components of the virus during the three hours it can survive in the airstream of a hospital.
In their Position Paper, ASHRAE also recommends multiple interventions in controlling the spread of infection.3 They state that healthcare facilities should consider improved particle filtration for central air handlers as well as upper-room or other UV interventions to control the inadvertent spread of infection and disease. This will be a combined effort through improved facility filtration and air treatment, as well as continued vigilance by housekeeping and personnel to disinfect surfaces and hands regularly.
For more information about BHB’s experience relevant to this topic, or if you have any questions, please don’t hesitate to reach out to us at mail@bhbinc.com.