The virus responsible for the COVID-19 disease, officially named SARS CoV-2, is very contagious and has quickly spread globally. The CoVs have become the major pathogens of emerging respiratory outbreaks in the world (Astuti & Ysrafil, 2020) and preventing transmission of the disease in our community is our best weapon against the outbreak. Transmission of the disease in an office environment can be mitigated through several means, listed below in order of increasing effectiveness and cost of implementation.
Physical Distancing and Barriers
The spike glycoprotein that forms the outer structure of the virus has a molecular weight of 150kDa (Astuti & Ysrafil, 2020), which is heavier than air. Unsupported molecules of the virus will drop out of the airstream due simply to gravity. Particles of the virus that are in solution with respiration moisture from an infected person’s lungs or mucus as part of a cough or sneeze could remain in the air for some time, depending on the velocity of the cough or sneeze.
Considering standard respiration, CDC guidelines are to maintain a six-foot minimum separation between occupants. This should be followed in general practice to allow any potential virus molecules to fall out of the air and land on nearby surfaces. Where this is not possible due to workstation proximity, partitions should be used between occupants. The partitions should extend vertically to at least 82” for standing desks, with the potential addition of transparent thermoplastic (plexiglass or acrylic) sneeze barriers on top of existing partitions to extend above the breathing zone and still allow light through.
Office personnel should minimize any contact with nearby officemates, and especially be aware of any surfaces that they touch outside of their area that may be infected. This will offer the best prevention against viral spread.
Filtration
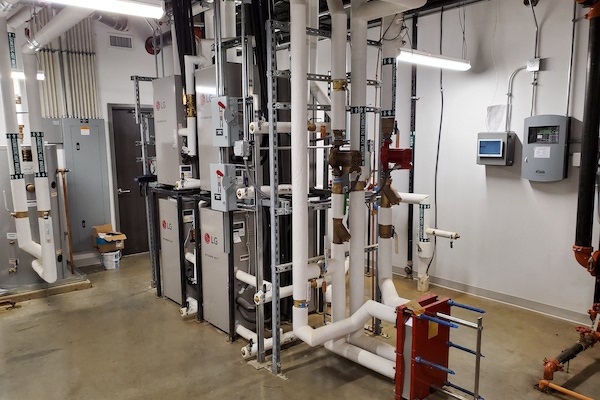
Where physical separation is difficult and where particles are potentially airborne beyond six feet, we can rely on the HVAC system to capture airborne particles and transport them back to the air handling equipment.
Traditional office design for HVAC systems utilizes ceiling supply and ceiling return, and the systems are designed to motivate mixing in the space to minimize any thermal gradients, or temperature differences, in the space. Per ASHRAE Standard 170, this type of system can also be utilized in an infectious isolation room. Ideally, airflow would be directed from high supply to low return so the cleanest air is in the breathing zone and the dirty air is low in the room, but this is not essential for capturing airborne particles from facilities. If particles of the virus remain airborne past six feet, then high return can pick them up and draw them into the return ductwork or the plenum. On the path back to the air handling equipment, some particles may drop out of the air and die on whatever surface they land upon, or they can potentially travel back to the HVAC system. If particles fall out of the airstream while in the ductwork, then fully developed flow in ductwork actually has zero velocity at the surface of the ductwork. This means that heavy particles that fall out will land on the duct surface and stay there. After approximately five days on the duct surface, the SARS-CoV-2 virus is expected to die and would pose no additional threat.
The SARS-CoV-2 virus is heavier than air and is not likely to travel long distances in the airstream, but future coronavirus outbreaks may have a lighter virus that can be suspended in the air longer. Once back at the air handling equipment, we can use other measures to trap and/or kill the virus.
For existing facilities, it is not likely that you will be able to add high efficiency (HEPA) filters. HEPA filters are physically bigger and have a higher pressure drop associated with them; this would require a larger air handling unit and a bigger fan/motor to move air through it. Air Force research on virus penetration through HEPA filters also concluded that particles of the virus will make it through the filter (Heimbuch, Wu, & Wander, 2009). The size of the virus that showed the highest potential for penetrating a HEPA filter was in the 0.1 micrometer range, which is approximately the size of SARS-CoV-2.
For existing air handling units, it is then recommended to utilize the best filter that can be accommodated by the existing equipment. MERV 11 filters offer a 65% filtration efficiency and would be considered good for commercial applications. Where MERV 13 filters can be installed, these would offer better performance with a 90% filtration efficiency and 98% arrestance for droplet nuclei. In this particular case, there would be marginal improvement to refitting existing equipment with HEPA filters and the improvement does not eliminate any threat of particle penetration or new infection.
In common areas or high-traffic areas of an office, it is possible to install fan filter units with HEPA media installed that will continuously filter the air. At increased air change rates (greater than 6 ACH), it is possible to turn the air over every 10 minutes and slowly decrease the potential amount of contaminant in the air.
Filtration does not kill virus particles that land on surfaces, so care will be needed during replacement of filters. Filters should continue to be replaced quarterly, or more often if your particular environment is dusty or dirty.
Dilution
The use of outside air to reduce the concentration of contaminants in buildings has been used effectively since the 1980s when Sick Building Syndrome became better understood. Building designers and engineers were able to find a balance (with the help of organizations like NIH, EPA, and ASHRAE) between a healthy environment and energy usage. The more outside air we bring into a building, the more energy we need to use to condition and filter that air.
In the case of Sick Building Syndrome, as well as infection control, increasing the amount of outside air introduced into a building for dilution will not remove the contaminant or the risk to individuals, it will just reduce the likelihood of new sickness or infection. Using models of airborne infections we can look at the impact of increased ventilation (ASHRAE, 2020).
Studying the model presented by ASHRAE in their Position Paper on Airborne Infectious Disease, as the amount of dilution air (or filtration of the air) that is introduced to the space increases, it shows diminishing returns. What this means is that going from 10% outside air to 20% outside air is effective in reducing the potential rate of new infections by about half (if everything else stays constant), but continuing to increase the amount of outside air (even up to 100% outside air) has much less of an impact. This is likely due to the fact that the potential source of infection is in the building.
Mechanical systems are designed to balance pressure and airflow in buildings, and to correctly treat the outside air in terms of heating, cooling, and humidity control. Since increasing outside air in existing facilities may not offer a significant improvement in the rate of new infections in the building, it is suggested that facility owners study the impact of increased ventilation on their building before making adjustments to system settings. The consequences could be pressure control problems in the building due to more supply than exhaust or return air, increased energy usage to treat the additional outside air (and in some cases existing equipment may not be capable of meeting the new loads), and potential humidity control issues in the facility.
Where additional outside air is needed, for new buildings or existing buildings that may not have proper ventilation today, a dedicated outside air system (DOAS) can be used to provide the space with higher dilution air rates. These systems can be retrofitted into existing buildings, but space limitations for equipment and new ductwork may be a challenge, as well as cost of implementation.
Dilution will not eliminate the virus, but it will decrease the number of new infections. Furthermore, this method is energy intensive as outside air is costly to condition.
Humidification
Recent research on the virus has shown that keeping humidity levels between 40-60% relative humidity (RH) can help to prevent viral transmission as well. (Moriyama, Hugentobler, & Iwasaki, 2020). Dry air allows the virus to travel through the air more easily, and conversely air that is too moist (higher than 80% RH) will cause the virus to drop out of aerosols more readily onto surfaces.
HVAC systems in comfort cooling applications tend to dehumidify air in the cooling season as a secondary benefit but are not usually controlled to maintain a specific humidity level. Traditional HVAC systems tend to keep the relative humidity below 60% in the cooling season, but humidification would be needed to keep it above 40% in the heating season and perhaps year-round for arid climate zones. Humidification can be achieved through steam generators with dispersion in ductwork and humidity sensors in the occupied spaces. This system can be retrofitted into existing buildings, but the steam generators may require reverse-osmosis or deionized water and drainage will need to be considered as well.
Decontamination
UV-Air
The virus has been shown to be sensitive to UV radiation. UV-C lamps can be installed in ductwork and at air handling equipment coils to kill the virus. However, this method will only work on droplets smaller than 5 micrometers and will not kill the virus that lands on surfaces. Furthermore, the virus needs to be exposed to the UV radiation multiple times to be neutralized, as the air may pass through the lamps too quickly to kill the virus on the first pass. Review of each unit will need to be done, along with the required intensity of the UV lamps, to ensure they are sized for the demand.
UV-Surfaces
UV lamps can be installed in the occupied space to routinely sterilize the space, but this method is disruptive as occupants will need to be evacuated. Furthermore, many materials in the indoor environment are susceptible to damage by UV radiation. This is more commonly utilized in healthcare environments where staff ensure there are no occupants in a patient room and UV light is used as an additional measure to clean the room between patients.
Potential Future Method: Ozonation and Ionization
Ozone can potentially be used to neutralize the virus, but studies have not been performed to verify this. However, Ozone has been shown to neutralize other similar coronaviruses such as SARS-CoV-1 (responsible for the SARS epidemic) and MERS-CoV (responsible for the 2012 MERS outbreak). (Elvis & Ekta, 2011)
Ozone generators could be used in the occupied space to neutralize the virus, but occupants need to be evacuated until Ozone levels in the occupied space fall below the Occupation Safety and Health Administration’s (OSHA) limit as Ozone is a toxic gas. (US EPA) It is an unstable chemical that will break down into regular, breathable oxygen, but it also interacts with volatile organic compounds (VOCs) found in the indoor environment to produce aldehydes and other toxic compounds. (Rai, et al., 2014) These compounds would need to be neutralized with ionization products.
It could be costly to implement this hypothetical method as monitoring of ozone and other by-products is necessary to maintain a safe working environment. Furthermore, this method will require that occupants be away from their workstations for varying amounts of time to implement, likely a minimum of two hours.
Conclusion
A prerequisite to any strategy discussed in this paper is a well-designed and maintained HVAC system. Each facility will be different, and each implementation of infection control will be different. We have seen for this particular virus (COVID-19) that droplet transmission seems to be the primary form of transmission. Once good housekeeping and hygiene techniques become commonplace, then we move to improvements in HVAC systems to reduce potential for airborne transmission. Future viruses or diseases that enter our work environments may have strong airborne components (as seen in the 1986 outbreak of H1N1) or very little (such as in the 2009 outbreak of H1N1).
To analyze your building and HVAC system and the impacts of SARS-CoV-2, please reach out to any of our mechanical engineers or mail@bhbinc.com for help or advise.